Machine learning (ML) in healthcare equips medical professionals with faster diagnostic insights and data-driven treatment options. It also helps patients receive timely interventions and more precise care plans. By identifying patterns invisible to the human eye, ML addresses clinical challenges that traditional methods cannot.
In healthcare, some of the biggest breakthroughs are happening in algorithms. A doctor takes up to 30 minutes for a full diabetic eye exam. Google developed a deep learning algorithm, ARDA (Automated Retinal Disease Assessment), that can analyze an eye scan for diabetic retinopathy within 20 to 60 seconds. Using 130,000 retinal photographs of diabetic retinopathy patients, Google’s ARDA helps doctors save time, enhance accuracy, and give patients faster results. Similarly, DeepMind’s recurrent neural networks predict Acute Kidney Injury (AKI) up to 48 hours before it occurs with 90.2% accuracy.
Machine learning helps healthcare professionals enhance their capabilities. It helps
-
Radiologists detect abnormalities faster with predictive analytics.
-
Primary care physicians make early interventions by integrating predictive analytics into electronic health records.
-
Critical care teams respond proactively with real-time patient monitoring.
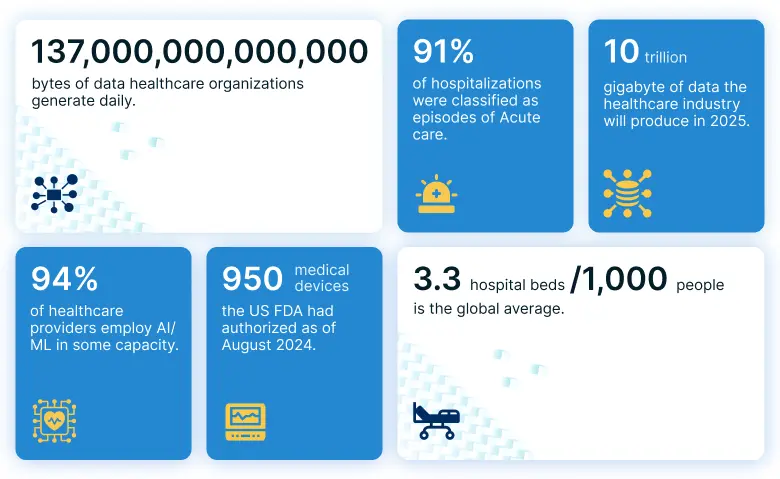
Machine learning services is highly used because today healthcare organizations have data in abundance.
Sources: HealthTech Magazine, the DATCON index, World Bank Group, AIHW, NCBI, Morgan Stanley Research survey.
This blog post explores how machine learning in healthcare empowers professionals to act faster and with greater precision. It features proven benefits, real-world applications from leading medical institutions, and actionable insights for healthcare organizations.
What is machine learning in healthcare?
Machine learning in healthcare is the use of algorithms and data to improve medical decision-making, diagnosis, treatment, and patient outcomes. Machine learning algorithms process medical data to learn patterns, classify clinical conditions, and make predictions. This capability is crucial for addressing the growing volume and complexity of healthcare data. Healthcare data is unique because:
-
Data location: Much of the data is in multiple places
-
Data structure: The data is unstructured and structured
-
Data format: It’s not all digitized in healthcare
-
Data complexity: A high number of data variables makes it hard to prepare for ML models
-
Regulations: Keeping up with bodies and the government
In contrast to traditional healthcare data analysis, machine learning systems evolve as new data becomes available. Models refine themselves over time and achieve greater accuracy with continued learning. Machine learning in healthcare equips providers with data-driven insights and tools to improve diagnostic accuracy and operational efficiency. The technology supports personalized treatment plans, speeds up drug discovery, and streamlines healthcare operations. Together, these capabilities contribute to better patient outcomes.
Healthcare machine learning use cases
From traditional practices to AI-powered insights, healthcare is evolving fast. Machine learning is reshaping care delivery, enabling precision, speed, and smarter decisions.
Use case 1: Disease outbreak prediction
Goal: Healthcare systems require efficient resource allocation especially during outbreaks. Outbreak prediction can help healthcare organizations to prepare ICU beds, ventilators, and triage stations. During COVID-19, for example, the CDC used its Forecast Hub with machine learning models to predict surges and give providers time to prepare.
Machine learning process: The CDC’s Forecast Hub used 13 machine learning models. These models analyzed population health data, environmental factors, and social patterns to predict where and when outbreaks might occur. They also processed COVID-19 symptom data, such as cough, fever, sore throat, shortness of breath, and headache, to forecast surges.
Benefits: Predictions from the Forecast Hub helped healthcare organizations send staff and equipment to the areas that needed them most. They also enabled hospitals to stock up on supplies in advance and prepare extra capacity before surges occurred.
Use case 2: Early health deterioration detection
Challenge: Healthcare teams face the critical task of identifying at-risk patients before their condition worsens. Traditional monitoring depends on periodic nurse checks, yet critical changes occur between visits. Machine learning systems offer continuous, 24/7 surveillance, detecting problems early and helping prevent serious complications.
Machine learning process: Early warning systems analyze data from Electronic Health Records (EHRs) in real-time. Systems combine a patient’s medical history with current symptoms, vital signs, and lab results to identify patterns. Algorithms process this information hours before warning signs become obvious to clinical staff by scanning thousands of data points every minute.
Benefits: Machine learning early warning systems reduce mortality rate, shorten hospital stays, and enable earlier interventions. Timely alerts help prevent ICU admissions and direct clinical focus to patients needing urgent attention.
Use case 3: Medical imaging diagnosis
Goal: Radiologists review hundreds of medical images daily. Human interpretation of complex medical imagery poses challenges in maintaining consistency across large volumes of cases. Machine learning systems offer potential for faster, more accurate diagnosis across various medical imaging applications.
Machine learning process: Medical imaging AI systems train on vast datasets of medical scans from patients with various conditions. Training machine learning models include hundreds of thousands of medical images, ranging from eye scans to skin lesion photos, to teach systems how to distinguish between healthy and diseased tissue. Algorithms process images within minutes and highlight suspicious areas for specialist review.
Benefits: Machine learning enables faster image analysis while maintaining diagnostic precision, allowing healthcare providers to process larger volumes of cases efficiently. For example, AI systems for eye disease detection achieve 94% accuracy, matching top specialists’ performance. Remote diagnosis becomes feasible and medical professionals can focus their expertise on complex, judgment-intensive cases.
WHITEPAPER
Revolutionizing medical imaging with computer vision: A comprehensive guide

Use case 4: Virtual nursing and remote monitoring
Challenge: Traditional care models cannot provide continuous monitoring for every patient. Nursing staff face limitations in maintaining round-the-clock surveillance while managing multiple responsibilities. Virtual nursing systems address this gap. The system tracks recovery progress and medication compliance while supporting human nurses with routine tasks.
Machine learning process: Virtual nursing platforms link with patient monitoring devices and EHRs to track vital signs, medication schedules, and recovery milestones. Machine learning algorithms learn from thousands of patient interactions and recognize normal recovery patterns. Personalized patient education and medication reminders are delivered automatically, while human nurses receive alerts about concerning changes.
Benefits: Virtual nursing reduces call light usage by 35% while improving patient satisfaction scores. Systems help catch problems early and reduce readmission rates. Human nurses focus on direct patient care while AI handles routine monitoring and education. Patients receive more consistent engagement and feel more supported throughout recovery.
Use case 5: Drug discovery and research acceleration
Goal: Drug development is time, cost, and resource intensive process. Sometimes, it takes 10–15 years and cost billions for each approved medication. Many promising compounds fail during expensive clinical trials due to difficulties in predicting human responses early in the development process. ML offers pharmaceutical companies the opportunity to identify strong candidates earlier and forecast therapeutic potential before costly trials begin.
Machine learning process: AI platforms examine databases containing millions of molecular structures, patient genetic profiles, and clinical trial outcomes. Machine learning identifies patterns linked to successful treatments for specific diseases and pinpoint promising candidates. Models train on decades of drug development data, enable accurate predictions of drug safety, efficacy, and optimal dosing strategies for different patient populations.
Benefits: Machine learning in drug discovery shortens development timelines and boosts clinical trial success rates. Platforms accelerate the identification of viable compounds while filtering out those likely to fail, saving millions in development costs. Research institutions direct more resources toward treatments with the greatest potential for success.
Key benefits of healthcare machine learning implementation
Machine learning provides opportunities to help assist medical professionals and staff, shorten time-to-care, and provide patient services 24/7.
-
Enhanced clinical decision-making
Machine learning algorithms quickly analyze large datasets to provide actionable insights at the point of care. They compare a patient’s data with extensive medical records to diagnose conditions faster and with greater accuracy. They give clinicians clear, evidence-based recommendations, reduce uncertainty, and improve patient outcomes.
-
Operational cost reduction
Machine learning algorithms process historical data and real-time metrics to identify inefficiencies, forecast equipment maintenance requirements, and streamline supply chain management. These systems provide administrators with data-driven strategies to reduce operational expenses while maintaining quality care standards.
-
Improved patient safety
Machine learning models continuously monitor patient vital signs and clinical indicators to detect any warning signs of deterioration or adverse events. They compare individual patient profiles against vast databases of similar cases. These intelligent monitoring systems alert healthcare teams to potential safety risks, enabling timely interventions.
-
Streamlined administrative tasks
Machine learning applications analyze administrative patterns to optimize appointment scheduling, reduce paperwork burdens, and eliminate redundant data entry processes. These systems free healthcare professionals from time-consuming clerical duties and allow them to dedicate more attention to direct patient care.
-
Personalized treatment approaches
Machine learning algorithms analyze individual patient characteristics, including genetic profiles, medical history, and treatment responses, to recommend tailored therapeutic strategies. They compare patient data against comprehensive databases to identify the most effective treatment protocols for specific conditions and patient types. ML enables clinicians to deliver precision medicine that maximizes treatment success.
A step-by-step process to applying machine learning in healthcare
Applying machine learning in healthcare works best when it follows a structured process. A stepwise approach ensures that every stage delivers measurable impact. This process speeds up deployment, maximizes clinical relevance, and return on investment.
-
Step 1: Identify and define clinical scenarios
To successfully implement machine learning in healthcare, organizations should first identify clinical scenarios. When evaluating clinical or operational applications, consider factors like:
- A clear gap between current and desired results. For example, the ability to identify high-risk patients within minutes.
- Health problems that can cause serious harm or death, such as those linked to late cancer screening or delayed detection of Acute Kidney Injury (AKI).
- The probability that available data and ML algorithms can enhance performance. For instance, models like random forest or gradient boosting (XGBoost) combined with preoperative and intraoperative data can improve AKI risk prediction in elderly orthopedic patients.
Clinical and data science teams collaborate to define measurable outcomes for these scenarios. Taking this step early ensures technical capabilities align closely with the realities of healthcare delivery.
-
Step 2: Establish data infrastructure and framework
Standardize and curate a schema that streamlines data into a unified structure. For example, a table organized by entities such as patients, visits, diagnoses, medications, and laboratory results. Structured data supports querying of longitudinal patient records and facilitates feature extraction for ML. The framework should feed ML pipelines with daily batch processes of patient and organizational data streams and APIs. Such constant data flow loads into centralized cloud storage and makes data available for consumption.
-
Step 3: Create Machine Learning Operations (MLOps)
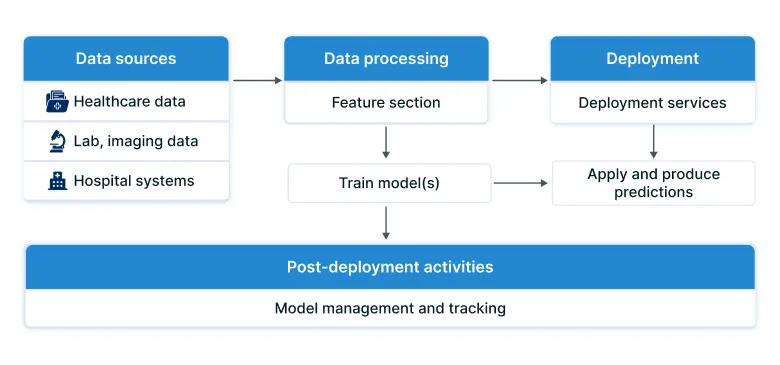
MLOps is a paradigm that integrates best practices from ML, software engineering, and data engineering to take ML models to production. The following image shows the end-to-end MLOps architecture in healthcare environment. Key MLOps principles include automation, orchestration, modularity, versioning, reproducibility, and monitoring.
-
Step 4: Continuous monitoring
Ongoing monitoring helps prevent model deterioration that can occur when patient populations, healthcare practices, or operational conditions change. Efforts should focus on clinically meaningful metrics, such as sensitivity and specificity, with clear thresholds for when adjustments are needed. Comparing input data, feature quality, and model predictions against trusted reference datasets enables early detection of disruptive shifts.
-
Step 5: Integrate models into clinical workflows
Bringing machine learning into clinical workflows calls for a structured, end-to-end strategy. Model outputs can directly trigger actions or provide clinicians with insights to guide their decisions. Alert pathways and care processes must be well-defined, ensuring the right person receives the right information at the right time. For non-urgent alerts, centralized teams can coordinate follow-up actions. Standardized care pathway documents help clinicians respond consistently, drawing on shared expertise and agreed-upon best practices.
Advanced ML technologies revolutionizing healthcare
From image-based diagnostics to predictive analytics, machine learning technologies are reshaping how care is delivered. These technologies offer faster, more accurate insights that help clinicians act earlier and with greater confidence.
-
Neural networks and deep learning
Neural networks identify subtle abnormalities in medical scans through pattern recognition algorithms. Convolutional networks analyze medical images using layered feature extraction with precision exceeding traditional diagnostic methods significantly. Retinal photograph analysis systems detect eye diseases through automated lesion mapping with remarkable sensitivity, enabling early intervention. Healthcare organizations report substantial improvements in diagnostic accuracy and reduced false positives.
-
Natural language processing
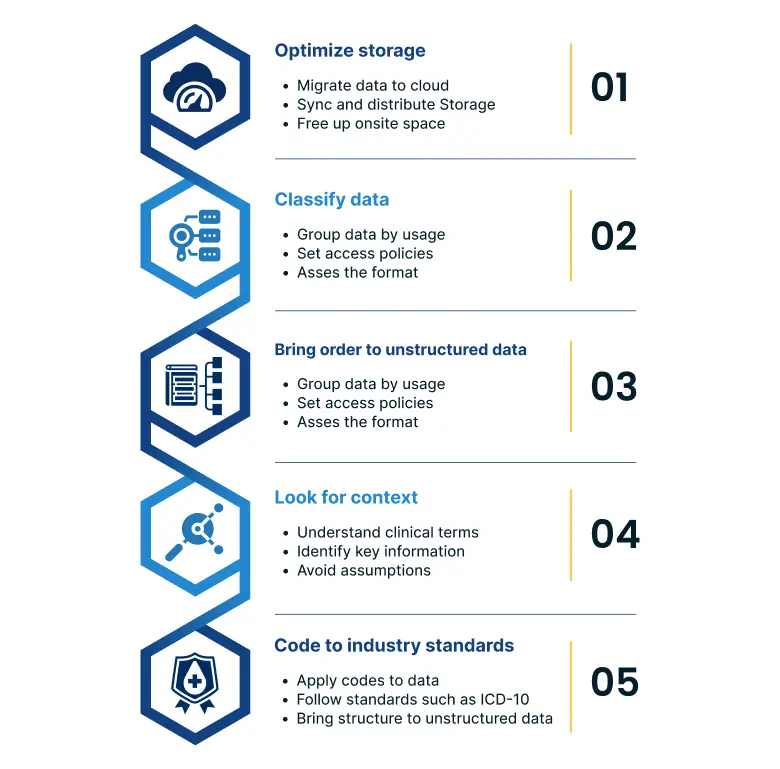
Natural language processing transforms unstructured medical text into actionable clinical insights through tokenization, entity extraction, and semantic analysis for organizations. The process of making unstructured data readable for analytics or ML models involves the following steps.
-
Robotic process automation
Robotic process automation manages insurance verification and appointment scheduling through rule-based workflows. It automates prior authorization with form completion and API integrations, so tasks that took days now take minutes and still meet compliance. It also streamlines billing and medication refill requests through intelligent document processing and database integration, reducing costs and improving processes.
-
Computer vision
Computer vision analyzes tissue samples for diagnosis using deep learning models trained on histopathological datasets. Automated feature detection and classification speed up large-scale screening programs, while ensemble models support early disease detection. Implementing these pipelines increases screening capacity and strengthens clinical workflows.
Machine learning algorithms used in healthcare
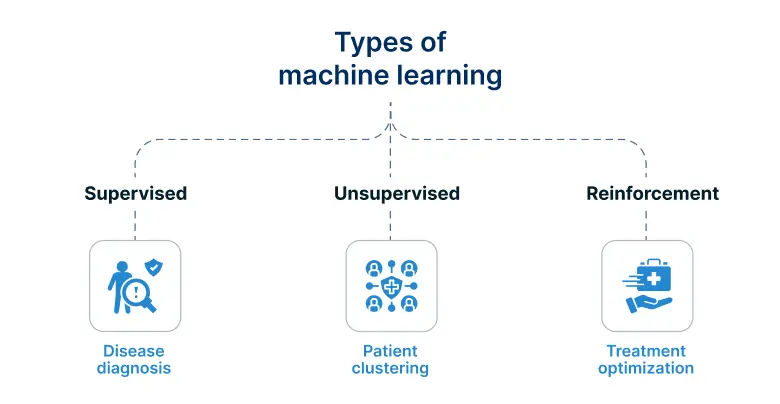
Machine learning algorithms in healthcare fall into three primary categories: supervised learning, unsupervised learning, and reinforcement learning, each serving specific medical applications.
-
Supervised learning
Supervised learning algorithms excel in diagnostic applications where historical patient data trains models to classify diseases and predict outcomes. Random forest algorithms predict sepsis onset with 94% accuracy. Support vector machines diagnose cardiovascular disease with 91% precision across varied patient populations.
-
Unsupervised learning
Unsupervised learning algorithms identify hidden patterns in medical data without predefined outcomes. K-means clustering groups patients with similar genetic profiles to guide personalized treatment. Principal component analysis simplifies complex genomic datasets by reducing them to manageable dimensions. These algorithms enable the discovery of new disease subtypes and treatment response patterns undetectable through traditional methods.
-
Reinforcement learning
Reinforcement learning algorithms optimize treatment protocols by learning from patient responses. Particularly valuable in chronic disease management, these systems adapt continuously based on patient progress and side effects. DeepMind’s reinforcement learning system optimizes radiation therapy dosing, reducing healthy tissue exposure by 30% while maintaining effectiveness.
Healthcare organizations implementing multiple algorithm types report synergistic benefits. Different algorithms complement each other to provide comprehensive medical insights.
Real-world examples of machine learning in healthcare
The following examples show the growing impact of machine learning in healthcare. They demonstrate how it improves patient outcomes, increases efficiency, and enables more personalized care.
-
Mayo Clinic: Predictive analytics for cardiac surgery
Mayo Clinic’s machine learning system analyzes over 50 variables from patient records, imaging studies, and lab results. With 95% accuracy, the system predicts cardiac surgery outcomes. Processing 10,000 procedures annually, the approach identified unknown risk factors and reduced mortality rates by 35%. Personalized risk assessments are also provided, helping patients make more informed decisions. Mayo Clinic’s success demonstrates how machine learning applications in healthcare can transform high-risk surgical specialties.
-
IBM Watson Health: Oncology treatment optimization
Memorial Sloan Kettering Cancer Center partnered with IBM Watson Health to create an AI system for cancer care. The system analyzes cases and recommends treatment protocols using the latest medical literature and institutional expertise. Processing over 1,500 cancer cases monthly, the platform delivers evidence-based recommendations that factor in patient-specific details and genomic profiles. Treatment plan concordance rates improved by 96%, while oncologist decision-making time dropped from hours to minutes. Adoption by more than 230 healthcare institutions worldwide shows the scalability of machine learning in specialized medical fields.
-
Google DeepMind: Diabetic retinopathy screening
Google DeepMind created a machine learning system that diagnoses diabetic retinopathy from retinal images with accuracy surpassing human specialists. The system has screened more than 100,000 patients in India and Thailand, detecting sight-threatening conditions in underserved areas with limited specialist access. Over 5,000 cases of blindness were prevented, and screening costs fell by 80% compared to traditional programs. The implementation demonstrates how machine learning can expand specialist-level expertise to resource-limited healthcare environments.
-
Stanford University: Skin cancer detection
Stanford’s machine learning platform identifies skin cancer from smartphone photographs with 91% sensitivity. Clinical trials show the system detects 30% more malignant lesions than primary care physicians, enabling earlier interventions and improved survival rates. The success illustrates how machine learning can extend specialized diagnostic capabilities to primary care and remote settings.
-
University of Chicago: Sepsis prediction
The University of Chicago Medicine developed a machine learning platform that predicts sepsis up to six hours before clinical signs appear. Drawing from over 100,000 hospitalizations, the system analyzes vital signs, lab results, and clinical notes to identify at-risk patients. Implementation reduced sepsis mortality rate by 18% and shortened hospital stays by 1.5 days. The results highlight the potential of real-time machine learning to prevent medical emergencies and improve outcomes in acute care.
These are just a few examples of the many ways machine learning is helping healthcare professionals. As ML technology continues to advance, we can expect to see even more innovative applications emerge.
Machine learning in healthcare implementation challenges and how to solve
Implementing machine learning in healthcare touches data integrity, regulatory compliance, and system interoperability. Without addressing these barriers, any ML system can fail to deliver clinical value. By pairing technical innovation with strong governance, ethical safeguards, and integration strategies, healthcare organizations can turn potential roadblocks into measurable outcomes.
-
Data privacy and security compliance
Challenge: Healthcare organizations face strict privacy rules under HIPAA, GDPR, and similar regulations. Patient data must remain secure while enabling training and deployment across systems. Sharing data for research or cloud AI solutions adds significant compliance complexity.
Solution: Federated learning trains models without centralizing patient data, preserving privacy. Algorithms learn from distributed datasets while ensuring regulatory compliance. Organizations using federated learning report 90% lower compliance risk and performance equal to centralized approaches.
-
Algorithm bias and fairness in medical AI
Challenge: Machine learning can amplify biases in healthcare data, affecting treatment recommendations. Insufficient diversity in healthcare data can cause AI models to perform poorly for some patient groups. Such biases risk worsening existing healthcare disparities.
Solution: Bias mitigation strategies span dataset diversification, fairness testing, and demographic performance monitoring. These measures improve model fairness by 85% and boost accuracy for underrepresented groups by 40%, ensuring more equitable healthcare outcomes.
-
Clinical integration and workflow adoption
Challenge: Healthcare professionals may resist AI tools disrupting clinical workflows. Poor interface design, alert fatigue, and inadequate training hinder adoption. Low utilization rates often occur despite proven technical capabilities and potential patient care benefits.
Solution: Human-centered AI augments decision-making and integrates with electronic health records. Training programs and phased implementation build staff confidence. Adoption rates reach 95%, with workflow efficiency improving by 75% in successful deployments.
-
Regulatory approval and validation
Challenge: Healthcare AI requires rigorous validation and regulatory approval, often delaying deployment for years. FDA requirements evolve rapidly, creating uncertainty. Innovative applications face added hurdles where no established validation frameworks exist.
Solution: Early engagement with regulators clarifies approval pathways. Quality management systems ensure compliance from inception. Proactive strategies cut approval times by 60% and achieve over 90% first-time approval success rates.
Turn your AI vision into action
Implementing machine learning in healthcare requires careful planning, clinical insight, and execution methods tailored to your organization’s needs. Our healthcare AI experts guide you from defining strategy to full deployment. We ensure compliance, seamless integration, and improved clinical workflows that deliver measurable results.
From enhancing diagnostic accuracy to reducing costs and accelerating research, our proven approach addresses privacy, validation, and workflow adoption challenges. We design machine learning solutions that improve patient outcomes and position your organization for lasting success.
Frequently asked questions
1. What is machine learning in healthcare?
Machine learning in healthcare uses AI algorithms to analyze medical data, improve outcomes, and streamline operations. Systems learn from patient records, imaging, and research to deliver predictive insights, decision support, and applications ranging from diagnostics to personalized treatment plans and operational optimization.
2. How is machine learning different from traditional data analysis in healthcare?
Traditional analytics applies fixed rules to historical data. Machine learning adapts continuously, detecting complex patterns beyond human recognition. Accuracy improves with experience. Models can process text, images, and numerical data to provide comprehensive insights for diagnosis, treatment, and operational decisions in healthcare.
3. What is the future of machine learning in healthcare industry?
Future healthcare AI will deliver real-time decision support, personalized treatments based on genetic data, and autonomous diagnostics. Predictive models will prevent diseases before symptoms emerge. Robotics will handle routine procedures, while precision medicine and efficiency gains will reduce costs and expand access to specialist expertise.
4. Can machine learning replace doctors?
No, machine learning supports, not replaces, doctors by providing insights and advanced pattern recognition. Physicians remain essential for complex judgment, patient communication, and ethical decisions. AI-augmented care combines technology with human expertise to enhance outcomes, improve efficiency, and strengthen clinical decision-making across medical environments.
5. Is patient data safe with ML systems?
Modern ML platforms protect patient data through encryption, strict access controls, and HIPAA/GDPR compliance. Federated learning enables training without centralizing sensitive data, preserving privacy while maintaining accuracy. Well-designed systems achieve 99.9% security rates, ensuring healthcare organizations meet high standards for patient information protection.
6. How does AI reduce costs in healthcare?
AI reduces costs by improving efficiency, detecting diseases early, and optimizing treatments. Machine learning prevents expensive complications, cuts diagnostic errors, and manages resources intelligently. Comprehensive AI adoption can lower operational expenses by up to 35% and reduce per-patient treatment costs by 20%.
7. What is the aim of AI and ML in healthcare?
The aim is to improve outcomes and reduce costs through predictive analytics and precision medicine. Machine learning accelerates research, broadens access to high-quality care, reduces clinician burnout through automation, and shifts healthcare toward proactive rather than reactive patient management on a global scale.
8. What type of AI is used in healthcare?
Healthcare uses machine learning for predictions, natural language processing for documentation, computer vision for imaging, and robotics for surgery. Deep learning analyzes complex scans, and neural networks process genomic data. Hybrid AI systems combine these technologies to provide comprehensive healthcare solutions.